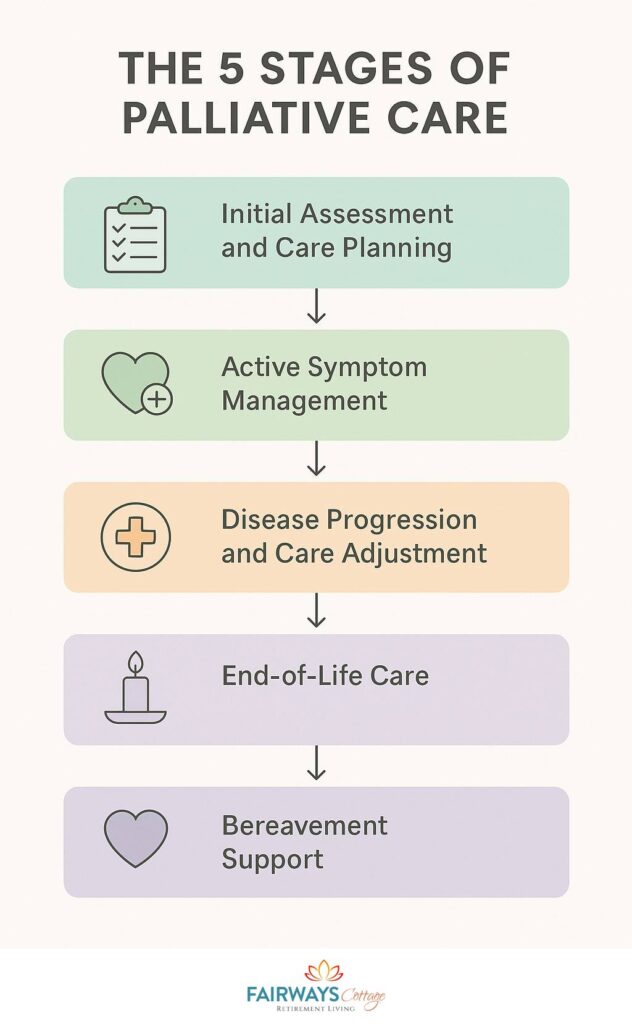
5 Stages of Palliative Care
If someone you love is facing a serious illness—or if it’s you—chances are you’ve heard the term “palliative care” tossed around by doctors, nurses, or social workers. But what does it really mean? And what does the road ahead look like?
Let’s be honest: this journey can feel overwhelming, especially in the beginning. There are new faces in white coats, unfamiliar words on discharge papers, and a quiet fear nobody quite knows how to name. As a geriatric care manager, I’ve sat beside countless families in this exact moment—hearts full of love, heads full of questions.
Here’s what I can tell you: palliative care is not about giving up. It’s not about doing “nothing.” It’s about choosing care that focuses on what matters most to the person who’s ill. It’s about comfort, dignity, connection, and support—at any stage of a serious illness.
In this guide, I’ll walk you through the 5 stages of palliative care, step by step. Not just the medical part—but the human part, too. Whether your loved one is at the very start of their diagnosis or nearing the final chapter, this is your roadmap. It’s built with compassion, shaped by experience, and written for people like you who are doing their best in incredibly hard circumstances.
So take a deep breath. You’ve come to the right place. And you don’t have to figure it all out alone.
Stage 1: Initial Assessment and Care Planning
Every journey needs a starting point, and in palliative care, this is it.
Stage 1 begins when a person is referred to a palliative care team—whether that’s in a hospital, a long-term care facility, or even at home. At this point, the goal isn’t to start treatment plans or make big decisions right away. The goal is to pause, look at the whole person, and ask one of the most important questions: “What does a good quality of life look like for you?”
What Happens During This Stage
1. A Full-Picture Evaluation
This isn’t a rushed doctor’s visit where you get five minutes and a prescription. This is a compassionate, in-depth assessment that covers:
- Current symptoms and physical needs
- Mental and emotional wellbeing
- Social supports and caregiver concerns
- Cultural or religious beliefs
- Spiritual needs and values
The care team takes time to really listen—because understanding the person is just as important as understanding the illness.
2. A Circle of Support
Palliative care is never one person’s job. It’s a team effort. You might meet:
- Doctors and nurses specializing in pain and symptom management
- Social workers who understand insurance, home care logistics, and family dynamics
- Chaplains or spiritual care providers
- Therapists or counselors
- Sometimes, even volunteers who offer companionship, errands, or just a listening ear
The team works together, making sure no piece of the puzzle is missed.
3. Creating the Care Plan
Now comes the most empowering part: building a care plan that fits. Not a one-size-fits-all checklist—but a tailored plan built around your loved one’s goals.
Some people say, “I want to be well enough to travel once more.” Others say, “I just want to sleep through the night without pain.” Every plan looks different, because every person is different.
The care plan includes:
- Symptom management priorities (e.g., pain, nausea, breathlessness)
- Emotional or psychological needs
- Goals of care (e.g., returning home, avoiding hospitalizations, staying lucid)
- Support for caregivers
- Plans for future decision-making (advance directives, power of attorney, etc.)
4. Planning for the “What Ifs”
This is also the stage where conversations around advance care planning often begin. These can be difficult but are so incredibly important. Your team may ask:
- “If your condition worsens, what kind of interventions would you want—or not want?”
- “Who should make decisions on your behalf if you’re unable to speak?”
- “What does comfort mean to you?”
These questions are never asked to scare you. They’re asked to respect your wishes before a crisis happens.
“This stage is not about solving everything. It’s about setting the tone—about showing that your voice matters and that your care will be built around it.”
Stage 2: Active Symptom Management
Once the care plan is in place, we enter the most hands-on and ongoing phase of palliative care: managing symptoms. This stage is all about relief—relief from the pain, distress, and discomfort that can come with serious illness.
But let me be clear: symptom management isn’t just about controlling physical pain. It’s about caring for the whole person. Because when someone is in pain, can’t breathe well, or is consumed by anxiety, life starts to shrink—and our job is to gently open it back up again.
What Symptoms Are We Talking About?
Every person’s experience is different, but some of the most common symptoms addressed in this stage include:
- Chronic or acute pain
- Fatigue and lack of energy
- Shortness of breath
- Nausea or appetite changes
- Sleep disturbances
- Anxiety, depression, or emotional overwhelm
- Cognitive fog or changes in thinking
- Spiritual distress—yes, that’s a real and valid symptom too
How Are Symptoms Managed?
1. Medical Management
Palliative care teams are experts in treating complex symptoms that don’t always respond to traditional medications. They may use:
- Specialized pain regimens, including opioids and nerve-targeting medications
- Antiemetics for nausea
- Steroids to reduce inflammation
- Oxygen or breathing therapies
- Appetite stimulants or nutritional plans
The focus is always on what brings comfort with as few side effects as possible. And if something stops working? The team adjusts. Fast.
2. Psychological and Emotional Support
Serious illness brings more than physical challenges. It can stir up fear, guilt, unresolved trauma, or deep sadness. During this stage, mental health care is just as prioritized as physical health.
Support might include:
- One-on-one therapy sessions
- Family counseling
- Medication for depression or anxiety
- Guided imagery or relaxation techniques
- Time with a chaplain for spiritual questions or grief
Even a single honest conversation can lift a weight you didn’t realize you were carrying.
3. Integrative and Complementary Therapies
These aren’t “extras”—they’re vital tools. And for many people, they offer comfort in ways traditional medicine can’t always reach.
Common therapies include:
- Massage therapy to ease tension and improve circulation
- Music therapy to reduce anxiety or spark joy
- Art therapy to express emotions without needing words
- Pet therapy, which has been shown to lower blood pressure and improve mood
- Acupuncture for pain and nausea relief
“The goal here isn’t to cure the illness—it’s to remove the obstacles that keep someone from living well in spite of it.”
For the Family: Your Needs Matter Too
Caregivers often forget themselves in the midst of managing appointments, medications, and emotions. But this stage is also for you. Let your team know if you’re exhausted, confused, or need a break. Respite care and emotional support for caregivers is a built-in part of palliative care—and asking for it doesn’t make you weak. It makes you wise.
Stage 3: Disease Progression and Care Adjustment
No matter how carefully we plan, illness has a mind of its own. Medications stop working. New symptoms emerge. A good stretch of stability might give way to decline. And sometimes, a patient’s personal goals shift as they reflect on what truly matters.
This stage is about staying responsive. It’s about adjusting the sails as the winds change—without ever letting the ship drift unattended.
What Does This Stage Involve?
1. Ongoing Monitoring and Reassessment
Palliative care is not “set it and forget it.” At this stage, the care team remains deeply involved, regularly checking:
- How symptoms are responding to treatment
- Whether new issues have emerged
- If the patient’s physical or emotional condition has changed
- If family needs or living arrangements are evolving
You’ll often hear a palliative care provider say, “Let’s check in again next week.” It’s their way of saying, “We’re still here. We haven’t walked away.”
2. Adjusting the Care Plan
Changes in condition often require reworking the original care plan—sometimes slightly, sometimes dramatically.
This might mean:
- Increasing medication doses for pain or anxiety
- Transitioning from home care to inpatient support (or vice versa)
- Addressing new goals, such as focusing more on rest and less on mobility
- Reassessing feeding methods or hydration needs
- Revisiting choices about future interventions
None of these decisions are made in isolation. The team walks you through the pros and cons of each option—at your pace, in your language, without pressure.
3. Support for Complex Decisions
Sometimes, this stage brings impossible-feeling choices:
“Should we try another round of treatment?”
“Do we go to the hospital—or stay home?”
“Is it time to stop certain therapies?”
In these moments, the palliative team becomes a sounding board—offering not just medical advice, but emotional support, ethical guidance, and a calm voice in the storm. You are never left to guess or go it alone.
4. Strengthening the Communication Loop
As the illness progresses, communication becomes even more essential. Between doctors. Between caregivers. And most importantly, between the patient and their loved ones.
Open conversations help:
- Prepare for what’s coming
- Prevent medical surprises or hospitalizations
- Reduce fear through shared understanding
- Give loved ones the chance to say what needs to be said
“Palliative care doesn’t wait for a crisis to act. It evolves with you—gently, thoughtfully, and with deep respect for your changing needs.”

Stage 4: End-of-Life Care
This is the chapter most families quietly fear—even when they’ve been preparing for it. And let me tell you something straight from the heart: it’s okay to be afraid. But it’s also okay to hope for peace, comfort, and love during this time. That’s what this stage is all about.
End-of-life care doesn’t mean abandoning care. It means redirecting it—fully and completely—toward comfort. It means honoring the person, not just managing the illness. And when done well, this stage can be one of the most sacred, meaningful times in a person’s life.
What Happens in This Stage?
1. Transitioning to Hospice (If Not Already in Place)
Hospice care typically begins when a person is expected to have six months or less to live and chooses comfort-focused care over curative treatments.
Hospice can take place:
- At home
- In a specialized hospice facility
- In a hospital setting
- In a nursing home or long-term care facility
The key is that the environment is peaceful, the care is gentle, and every action supports dignity above all else.
2. Total Focus on Comfort
- Pain relief becomes the top medical priority. This may involve stronger medications, frequent adjustments, and round-the-clock monitoring.
- Symptoms like breathlessness, anxiety, confusion, or agitation are actively managed with thoughtful, compassionate care.
- Non-medical comfort is prioritized too: warm blankets, soothing music, gentle touch, familiar voices, and meaningful rituals.
“In this stage, care doesn’t end—it deepens. It becomes less about prolonging life, and more about enriching what time remains.”
3. Emotional and Spiritual Presence
As the body slows, the spirit often awakens in unexpected ways. Many people become reflective, peaceful, or deeply present.
Palliative and hospice teams provide:
- Access to chaplains, spiritual advisors, or faith leaders
- Space for forgiveness, gratitude, or closure
- Support for legacy-building—like writing letters, creating memory boxes, or recording messages for loved ones
This is a time when small gestures carry enormous meaning.
4. Family Involvement and Support
You are not just watching. You are part of the care team now.
- Families are encouraged to participate in bedside care if they wish—holding hands, offering water, applying lotion, sharing stories.
- The team prepares you for what to expect physically and emotionally as death approaches.
- You’ll also receive guidance on practical matters—like legal documents, funeral planning, and grief support options—so nothing is left to guesswork.
And perhaps most importantly: you are never alone. Hospice teams often offer 24/7 on-call support. They answer questions at 2 a.m. They sit beside you when the silence feels too loud. They stay.
“Death, when approached with care and compassion, can be a moment of connection, not just loss. It’s a final act of love—and it deserves the same gentle attention as every other stage of life.”
Stage 5: Bereavement Support
After a loved one dies, the house gets quiet—but your heart does not. The world expects you to move forward, but you may feel stuck between two realities: one where life continues, and one where everything’s changed.
That’s why palliative care doesn’t end with death. It continues for the people left behind. This final stage—bereavement support—is about walking with families through grief. Not to rush them. Not to fix what can’t be fixed. But to offer presence, tools, and care as they find their way.
What Does Bereavement Support Include?
1. Immediate Grief Counseling
In the days and weeks after a loss, emotions can feel overwhelming—shock, guilt, anger, numbness, even relief (which can bring its own guilt).
Hospice and palliative teams often offer:
- Phone calls from grief counselors or social workers
- One-on-one grief therapy sessions
- Crisis support if emotions become unmanageable
No one will judge how you’re grieving. There’s no right way to do this.
2. Support for Funeral and Memorial Planning
Even the most organized families can feel adrift during funeral arrangements. The team can help with:
- Understanding what legal documents are needed
- Choosing between burial, cremation, or other options
- Writing obituaries or preparing eulogies
- Coordinating with spiritual or cultural leaders for services
Some hospices even offer legacy services—guiding families in creating memorial scrapbooks, tribute videos, or letters from children to a lost parent.
3. Long-Term Grief and Healing Resources
Grief doesn’t stick to a schedule. That’s why most programs extend bereavement support for 12 months or more.
Available resources might include:
- Weekly or monthly support groups (virtual or in-person)
- Books and reading materials geared toward different types of loss (e.g., spouse, child, parent)
- Special programs for children or teens
- “Grief anniversaries” support—such as on the one-year mark, birthdays, or holidays
“Grief is not something you ‘get over.’ It’s something you grow around. And you don’t have to do that growing alone.”
4. Caring for the Caregiver
You may not even realize it yet, but caregiving changes you. It can bring exhaustion, loneliness, or even identity loss—especially after a long illness.
This stage also gently encourages you, the caregiver, to begin healing:
- Take a break without guilt
- Reconnect with your own health needs
- Talk about the experience with someone you trust
- Allow space for joy when it begins to return
You are not “moving on.” You’re moving forward—with love, memory, and maybe even a little grace.
Additional Resources
Because navigating palliative care often raises more questions than answers, I’ve put together this extended resource section to help you feel steady, informed, and connected—no matter where you are on this journey.
FAQs About Palliative Care
1. What’s the difference between palliative care and hospice?
This is the most common question I get—and for good reason. Here’s the simple answer:
- Palliative care can begin at any stage of a serious illness, even right after diagnosis. It can be provided alongside curative treatment (like chemotherapy, dialysis, or surgery). It’s about improving quality of life—whether someone is expected to live for years or months.
- Hospice care is a type of palliative care, but it begins when a person has a life expectancy of six months or less and decides to focus entirely on comfort rather than curative treatments.
Both are compassionate. Both are focused on dignity. The difference is timing and treatment goals.
2. Can children receive palliative care?
Yes. Pediatric palliative care is a specialized field designed to support children with serious illnesses—like cancer, genetic disorders, or neurological conditions—and their families.
It addresses:
- Pain and symptom management for children
- Family-centered decision-making
- Emotional support for siblings
- Help with schooling, developmental goals, and memory-making
No child is ever too young to deserve comfort and care.
3. What if my doctor hasn’t brought it up? Can I still ask for palliative care?
Absolutely. Palliative care is not something you have to wait to be offered—it’s something you can ask for.
Try saying:
“We’re feeling overwhelmed. Can we talk to someone about palliative support to manage symptoms and help us plan ahead?”
Most hospitals have a palliative care team or can refer you to community resources. If not, your primary care physician or specialist can help coordinate it.
4. Is palliative care only for cancer patients?
Not at all. Palliative care is for any serious illness, including:
- Heart failure
- COPD or chronic lung disease
- Alzheimer’s or other dementias
- Parkinson’s disease
- ALS
- Kidney or liver failure
- Stroke recovery
- Complications from chronic conditions like diabetes or autoimmune diseases
5. Will my insurance cover palliative care?
Most likely, yes. In the U.S.:
- Medicare and Medicaid typically cover palliative and hospice services
- Private insurance often does as well—coverage varies, so it’s worth a call to your provider
- Many nonprofits or hospitals also offer support regardless of ability to pay
If financial concerns are stopping you, ask for a palliative care social worker to help you navigate resources.
Glossary of Terms You Might Hear
Here are a few terms that often confuse or intimidate families. Let’s take away the mystery:
- Advance Directive – A legal document that outlines your care preferences if you become unable to speak for yourself. It can include a living will and medical power of attorney.
- DNR (Do Not Resuscitate) – A medical order stating that healthcare providers should not attempt CPR if the heart stops or breathing ceases.
- Comfort Care – Care aimed entirely at easing symptoms and distress without attempting to cure the illness.
- Goals of Care Conversation – A talk with your medical team about what matters most to you and how your treatment should reflect those wishes.
- Hospice – A form of palliative care focused on end-of-life comfort, generally for those with a prognosis of six months or less.
- Palliative Sedation – The use of medication to relieve severe, unmanageable symptoms when other methods have failed, typically near end of life.
- Respite Care – Temporary relief for caregivers, providing them with rest while a professional takes over care duties for a few hours or days.
- Interdisciplinary Team (IDT) – The core palliative care group (doctors, nurses, social workers, chaplains, etc.) that works together to support the patient and family.
Trusted Links and Support Networks
You don’t have to sift through endless Google results—we’ve gathered the most reputable, caregiver-approved sources right here:
For General Palliative Care:
- Center to Advance Palliative Care (CAPC) – Offers tools, provider directories, and patient resources.
- GetPalliativeCare.org – Patient-facing site to help you understand services, eligibility, and how to find care.
For Hospice Guidance:
- National Hospice and Palliative Care Organization (NHPCO) – The gold standard for hospice information, including a searchable provider directory and end-of-life planning tools.
- Hospice Foundation of America – Focuses on public education and grief support.
For Caregivers:
- Family Caregiver Alliance – Practical tips, emotional support, and state-by-state resource listings.
- CaringInfo – Free legal forms, advance directive templates, and state-specific end-of-life laws.
Grief Support & Bereavement:
- GriefShare – Find local grief support groups by zip code.
- What’s Your Grief – Offers articles, courses, and coping tools from licensed mental health professionals.
- Modern Loss – Candid, real-world perspectives on grief, especially for younger adults.
For Pediatric Palliative Care:
- Courageous Parents Network – An invaluable resource for families caring for children with life-limiting illnesses.
- Children’s Hospice International – Promotes integrated palliative care models for children worldwide.
If there’s a resource you wish existed or a topic you still feel unsure about, don’t hesitate to reach out in the comments or contact form. I’ll do my best to help—or point you to someone who can.
“Support isn’t just about care—it’s about knowing where to turn when you need a hand, a break, or just someone to tell you that you’re not alone.” — Margaret Grace
Conclusion
If you’ve stayed with me through all the five stages of palliative care, thank you. Not just for reading, but for showing up for someone you love. For seeking clarity in the middle of confusion. For trying to prepare, even when your heart might feel anything but ready.
Palliative care isn’t about counting days. It’s about making each day count—with comfort, with dignity, and with meaning. It’s a kind of care that listens more than it speaks, that adapts instead of insists, and that honors not just the body, but the human spirit.
Let’s quickly recap what we’ve covered:
- In Stage 1, we built a plan rooted in personal goals and values.
- In Stage 2, we tackled symptoms head-on, making space for comfort and peace.
- In Stage 3, we stayed flexible, adjusting care as the illness evolved.
- In Stage 4, we shifted into end-of-life care—offering grace, presence, and support until the very last breath.
- And in Stage 5, we stood beside grieving families, knowing that love doesn’t end when a life does.
You may be somewhere near the beginning right now. Or maybe you’re already in the hardest stage, navigating the days after a loss. Wherever you are, please remember: you don’t have to do this alone.
Use the resources. Ask the questions. Say the things that need to be said. And if nothing else, take comfort in knowing that compassionate care exists—care that centers your values, respects your decisions, and gently walks beside you through every turn in the road.
Share This Article: